Earlier I wrote that I use only two parameters with patients to show them where they are in therapy – and as periodontal patients they can only be in one of two categories. They are either in Active Therapy or Supportive Periodontal Therapy. To help them to know which treatment category they are in, I use two simple parameters, Bleeding Index and Advanced Sites.
In anticipation to someone’s push-back, let me make a few statements up front.
- These two categories are broad and generalized intentionally. Yes, I know. There are exceptions to the rules, but you can make these exceptions in your patient documents against what I consider some pretty reasonable norms. If you disagree that what I am saying here is generally true, then please do two things. First, let me know. I could be wrong and am willing to adjust to new information. Secondly, do what you believe to be true and establish your norms accordingly.
- Yes, I know there are other indices that are very useful and I am not so tunnel-visioned to simply rely on these two, however, when it comes to patient communication I think we always need to understand that loading patients down with too much information when it does not change or modify the overall message only adds to their confusion and increased inability to make the important treatment decisions they need to make. We end up spending more time in discussions than necessary, which eats into patient care somewhere else. So I opt to keep things simple in SPT. Also, when thinking about the subject of SPT, I am thinking about the management of many patients, not just one. This is part of the departure from dental school. Neither we nor patients can afford wasting appointment time trying to make simple determinations and give routine explanations to patients. All of this has to be designed into a process that the office executes daily. Keep in mind that before a patient is ever in SPT all of these concepts have already been explained. (We will get to the presentation on how to explain what periodontal disease is to patients shortly, but not today).
- It is important to remember that our discussion here is SPT not Active Therapy (I may start abbreviating this as AT in the future, so be ready). What is odd about this is that I have chosen to start with the end first. Most courses will work through diagnosis and treatment and finally get to the topic of maintenance. This makes it seem (at least to me) that it comes across to students, and later, patients as an afterthought. When the significance of SPT is underappreciated and the office response is tepid, patients stop coming when they should and yet they usually continue to believe that everything is fine. If they stay away too long, everything will start to unravel. Your front office people need to know this.
- I acknowledge that there is a down-side to writing things in the order that I have. It means that I am not discussing – and have not yet discussed – how we achieve this state in periodontal therapy. My assumption is that I am writing to people who have already studied all of this information before. In fact, I believe I am writing to dentists and dental hygienists who are currently engaged in treating periodontal patients. (If you are a dental student or hygiene student, welcome, you are ahead of the game. Feel free to share this with your instructors and classmates). This discussion, therefore, is intended to be more practical than theoretical. If my posts were to provide the initial lectures about periodontics to the uninitiated, I would have started at the beginning just like everyone else. This is not to say, however, that I wouldn’t introduce early in dental school clinics patients who are in SPT. Dental and hygiene students need to be shown early on what periodontal stability looks like following treated periodontitis because it doesn’t look like the periodontium of someone who has never had this type of chronic infection. Also, they need to understand what providing care for this unique population looks like. (It turns out to be quite simple, which makes this treatment a good clinical activity for sophomore and junior dental students).
- Finally, and this is beating a drum already beaten in earlier posts, I want it to become crystal clear to you that SPT is a level of sustained health, but one that contains the residuals of a chronic slowly progressive disease. It is vital for those assuming the responsibility for managing SPT that they are able detect and communicate when things are not working as hoped. Following this, they must then correctly treat whatever problematic change has occurred. When dental offices are not looking at SPT correctly and, therefore, not accomplishing the assessments necessary at each appointment to determine what patients need next, they are setting up conditions for unpleasant (and unnecessary) confrontations and/or desertions by patients. This is what happens when compliant patients after receiving an untold number of “cleaning appointments” with little documentation or feedback suddenly discover that everything is not OK. This is especially troubling when their first inkling of problems come after discovering for themselves progressive tooth mobility or periodontal abscesses.
Now on to Parameter #2 – Advanced Sites
There is a great deal of periodontal literature on the subjects of pocket depth measurement, clinical attachment, the microbiology of periodontitis, etc., etc. It’s important material for periodontists and other interested dentists as well as research scientists to know, but in order for any of this to have clinical usefulness, we need to condense it all down to some reasonably accurate and usable statements.
To me statements about periodontitis and periodontal therapy are useful when the following conditions are met:
- The statements are true (we aren’t making any of this up to “sell” patients anything), even though they may be incomplete – meaning there is a whole lot more to the story but that the additional detail doesn’t change the clinical realities.
- The statements help clinicians know what to do therapeutically.
- The statements are explainable to patients in ways that help them make decisions.
Here are a few statements about pocket depth in relationship to disease that I believe fit these conditions. With the exception of the information placed in parentheses, I will likely at some point share all of these facts with periodontal patients:
- In gingival health, pocket depths are 1-3 millimeters.
- Patient plaque control is effective, without help, at pocket depths between 1-3mm. (BTW: There is no such thing as a pocket depth of 0mm because measuring we always round up to the next number).
- Early periodontitis involves attachment loss and pocket depths that are at least 4mm. (In other words we are not just looking at enlarged or overgrown gingiva or gingival recession).
- Moderate periodontitis involves attachment loss and pocket depths that are up to 5mm.
- Advanced periodontitis involves attachment loss and pocket depths that are 6mm and deeper.
- The absence of bleeding upon probing is a good indicator that the site is stable. (The presence of bleeding in a single site is a weak indicator of progression of disease and is in part the reason why in the bleeding index I set the crossover from AT (Active Therapy) to SPT at 20%).
- Certain organisms within subgingival plaque are not present in periodontal health and have destructive (pathogenic) characteristics. They kill off the good bugs and reside where least disturbed, in pockets deeper than 5mm.
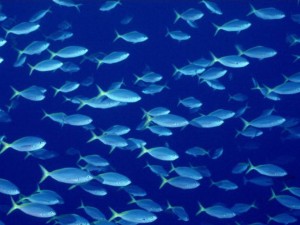
If they were fish in the ocean, this is what they would look like
As opposed to healthy plaque which would look like this
There is one additional statement I think is important to include because it provides clinicians with some measurement latitude.
8. Probing error is plus or minus one millimeter. This means that if I measure 3mm, it could be measured by me or someone else later as 2mm or 4mm. If a change of one millimeter in either direction is within probing error then evidence of true change, is 2mm or more. (Note that I said evidence of true change, not true change itself. This is because we can never know for sure that true change occurred or exactly why in a specific site. I know I’m beginning to sound like a physicist discussing the location of electrons around an atom, but we are seeing evidence of change and not the activity of change).
When probing error is added to the above statements, it means that early, moderate and advanced conditions are relative terms. This means you can modify your interpretation when it seems appropriate to do so. (For example, if someone has extremely short or blunted roots, 4-5mm pockets may be considered advanced because this patient has less of a cushion before tooth loss occurs.) Also I find it comforting to know that the more the measurements are repeated the more confident we can be that they accurately reflect the clinical situation. By the time someone is in SPT, having gone through AT, there will have been a number of pocket depth measurements performed. The greater our confidence that our measurements are accurate the easier it becomes to react to change when we see it.
OK. Let’s finally now reduce the information from the 8 statements above and condense them down to the three things patients need to understand.
- Advanced sites are pockets measuring 6mm or more.
- We do not like to see advanced sites in SPT because we no longer can predict with any confidence that they will remain stable between what we consider to be the shortest reasonable appointment intervals – every 3 months. (Let’s hold on a discussion about appointment intervals for another time).
- Six millimeter pockets are a problem because plaque converts to really bad bugs when pockets go from 5mm to 6mm.
Can someone stay in SPT with 6mm pockets? Sure, when the patient’s chooses to do so after understanding of risks, but 6mm is a flag that may indicate we need to return to a short phase of AT. This may simply be repeat light root planing and follow-up. The root planing may be with or without an anesthetic, depending. One thing is certain, however, if we are returning to AT, there must be a statement as to why.
I consider root planing to be outside of SPT, therefore a new diagnosis should begin the process to justify returning to AT even briefly. The dentist must be involved in this assessment and the record should so reflect. If this is not done, then the record becomes muddy and it will be difficult to explain to others what you are doing and why (I’m thinking insurance companies here as well as the patient when a change in cost enters the equation).
Well informed patients track the numbers and understand what they mean. They know that their bleeding index should be under 20% and that they should have no pockets greater than 5mm. When we boil this all down, how hard is that?
When the numbers reflect concerns, patients are then quickly able to decide what it is they want to do. Here are a few reasonable options that might be considered when deeper pockets recur:
- Maintain by light subgingival ultrasonic scaling for one more cycle of three months
- Place Arestin for one cycle only
- Repeat light root planing
- Periodontal surgery (regenerative or respective in nature)
- Something else
That’s enough for now. I’m close to finishing my thoughts on SPT. Thanks for the comments and questions received thus far. The dialogue really helps me gage whether or not the information is helpful and where further explanation might be of benefit.
If you are on Twitter, consider connecting. When you follow, please message me that you following me because of these posts. I will then follow back. I don’t automatically following back everyone who follows me. And through Twitter or other avenues, feel free to pass this information to others you think would benefit.
Next time I will get into what procedures are performed at the routine SPT appointment.